10 Minute Read
Our conversations tell us a lot about who we are, so we thought it would be a good idea to review our top list serve conversations for 2020. Before those of you who are not members of the Collaborative Family Healthcare Association (CFHA) stop reading, let me convince you as to why you should continue reading. In short, our conversations say a lot about the progress we have made in bringing physical and mental health together in the health system – and this is a harbinger of the change that is to come. So, stick with this for a bit.
Here are our top five conversations (longest threads) for 2020.
#1 Looking for Decision Tree for Complex BH patients
This conversation, like most, started out as a simple request. A member asked for a decision-tree that would help physicians determine the most appropriate level of care for patients.
“I’m not sure if it is related to COVID or something else, but we are seeing a recent influx of very complicated patients coming in to our system. In some cases, they really are not appropriate for our integrated care model and we are trying to develop a tool that will help PCPs determine whether the patient is a good fit for our BHCs or not. Diagnosis alone isn’t enough as there are too many exceptions to the rule. Does anyone have any decision trees or algorithms that could help with this? It ends up being a customer service nightmare when the PCP refers to the BHC and then the BHC has to tell the person they need a higher level of care than we can provide.”
And like many seemingly innocuous questions, our list serve blew up. The responses gave a stunning picture of how much we have learned about caring for patients with complexity and how important it is to think critically about what complexity means in relation to the system of care. In other words, “complex patient” does not automatically mean a referral out from primary care to specialty mental health care. A number of factors need to be considered including the patient’s/ family’s preferences, stage of change, the model of care employed in the clinic to name a few. In fact, the correct answer could be, “Yes AND…”
What would you do if these were patients who walked in to see the PCP and needed a (non-emergency) specialist? Would the PCP simply look at the patient and say, “I’m sorry I can’t help you. You need more intensive services.” ? Or would the PCP do something at the primary level to help that patient for the immediate future and before scheduling a follow-up or referring to a specialist? Whatever your answer is, that’s how the BHC should operate.
– said one respondent to the query.
Complexity is a key issue we integrators are addressing when working towards whole-person care. There is complexity on the patient side and the health system side. The depth of this conversation tells us that we are beyond foundational questions related to integrating behavioral health and physical health – we are now addressing the meta questions related to who and what primary care is and what teams are designed to do in the current system versus what they really should be aiming for in an ideal, reconfigured system of care. This is an issue the board President of CFHA, Dr. Andy Valeras has championed, for example.
#2 AMA Creating An Integrated Care Group
Ok, so this list serve conversation took off when members found out about an effort by the American Medical Association (AMA) to champion integrated care. Suffice to say that there was some consternation about why CFHA was not involved in the process and whether the AMA would sufficiently champion different models of integrated care not just models that served guild interests (eg. such as psychiatry). When the dust of the conversation settled we learned that CFHA had in fact had communication with the AMA and that at least one member of CFHA was involved in the process and that team-based care broadly-speaking was being highlighted as central to enacting integrated care.
What was interesting about this conversation is the notion that the community has a much clearer definition of integrated care and chafes at any efforts to take us back to the beginning when guild interests and models were in a pseudo-warfare against each other. It is clear that the Collaborative Care Model (CoCM) and the Primary Care Behavioral Health model (PCBH) and all of the clinical pathways that have emerged alongside these models like SBIRT and MAT have their adherents. But gone are the days when we blindly broad-brush integrated care as a monolithic thing or when we make claims about one model over another when each of these models have very different end-points and purposes.
PCBH and CoCM are starting points…to not start there for the BH components of primary care… in my mind isn’t practical… (quality and cost) and from those bases (and others like those in other fields) a new Interprofessional Primary Care can (and does frequently) rise.
– a respondent to the initial query.
#3 Collaborative Care Billing Question
Actually the next three top threads on our list serve were on this topic, so this is a conglomeration of those, which tells you something right off the bat: CoCM billing is still problematic. Well, billing for integrated care in general is problematic, but that’s a story for a different day. These threads highlighted the difficulties with knowing whether particular payers payed for the CoCM codes, whether they paid for some or all of them and confusion as to how to use these codes in conjunction with psychiatric diagnostic codes (commonly referred to as psychotherapy codes).
Clinics are clearly still figuring out how to bill for these codes which differ from standard office-visit codes since the codes capture time spent in other activities such as managing a registry and case consultation with a prescribing provider. Fortunately for our community the good folks at the AIMS Center frequently step into our conversations and provide guidance on how to approach these issues and here is a helpful guide about where things stand with the codes.
#4 Behavioral Health Diagnostic Assessment in Primary Care Behavioral Health
Should you perform psychological testing in primary care or not? That was the basic question being asked and boy did people have opinions. Few people were advocating for full-fledged psychometric testing services, but the community seemed to feel that testing could serve a function in some primary care settings without distracting from availability of services if directed well by the needs and goals of the primary care service and the community.
As one poster put it,
The scope of diagnosis and assessment should be limited to questions that will influence the delivery of an intervention that can be expected to improve outcomes. Stated more bluntly – there is limited value in clarifying a diagnosis if that clarification does not impact treatment. In most cases this is the standard the best primary care physicians use when making decisions about screening and assessment, and it is the standard that BH providers in primary care should be holding themselves to.
#5 Billing For H&B Codes and Screening Codes
The last of our top five threads for 2020 were also related to billing and coding questions. Specifically changes to the the Health and Behavior Codes (HBI) which revamped them to align better with the time-based nature of the older psychotherapy codes. Not everyone was a fan, given that one of the HBI codes use to allow for a 15-minute visit increment compared to the newer code which runs from 16 to 37 minutes, but we all found ways to work with them.
One poster summed up the discussion well, “The 30 minute visit codes go from 16-37 minutes as you have to reach the half time (8 minutes at least) to do the add ons. Ends up being the same time break downs as the psychotherapy codes (16-37, 38-52, and so on). They also increased the RVUs associated which should support improvement in reimbursement rates. Although I wish the initial code had remained at 15 minutes, they seem to have a lot of potential. I highly recommend the APA webinars: https://www.apaservices.org/practice/reimbursement/health-codes/health-behavior/webinar.”
Another similar thread focused on billing for administering screening instruments, which of course include a conversation about whether it was even worthwhile. One poster topped the conversation off with some sage advice:
It [whether it is worth billing] is dependent on multiple variables and I encourage folks to use the 5-step process (Healthcare Institution Site License (legalities), Site Type, Payers (stakeholders), Provider License Type (workforce), Service Delivery and Coding (business case) which has been presented and published/republished multiple times. If you use the process then you will be able to identify and design your billing structure, financing for integrated care, and workflows accurately… Please remember, that depending on the 5 steps, differing clinics may have differing billing, RVUs, and workflows based off of their state, license, site type, providers, etc.
In other words, whether it is possible and whether it even makes sense to bill for screening, depends…
Closing The Door On 2020
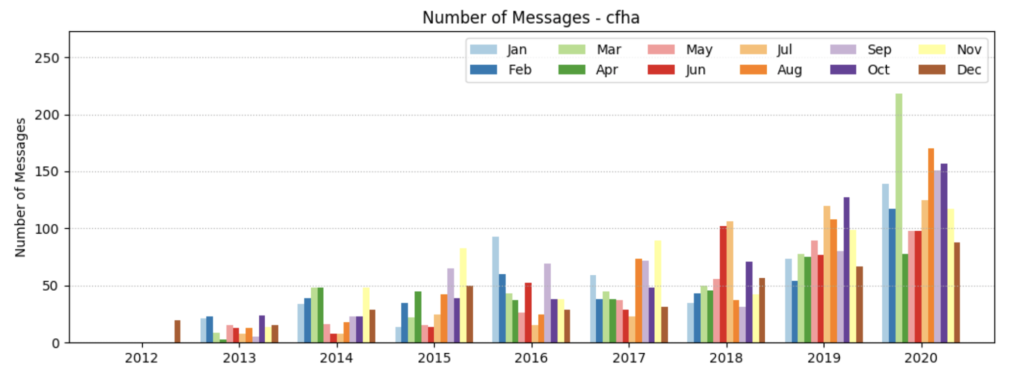
So, those were the top five longest threads of the year, but in truth much of our conversation, especially in the middle of the year, was around COVID and the workflow adaptations members were making on the fly. These were not necessarily long threads, but they were numerous as members shared workflow information with one another. In fact our highest ever list serve thread month was unsurprisingly March 2020 with 218 messages, most around COVID and telehealth adaptations.
The communication on our list serve reflects how far we have come and where we need to continue to work. Our level of sophistication around integrated care, team-based care and what works has increased dramatically. Our resilience in transitioning to virtual care clearly shows how well integrated behavioral health is in our member clinics. And, we also need to continue to work to impact policy, especially with regard to streamlining and aligning payment to the team-based services our members provide.
So there you go. 2020 seen through the eyes of CFHAs list serve. Let’s see how our conversations evolve in 2021!


Leave a Reply